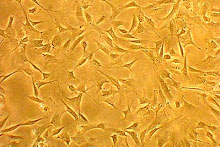
Several years ago, we introduced the concept of a "Progenitor Helper Cell". At the time, all that was known was that MSC's needed to be present to help other cells like blood stem cells (CD34+). Experiments had shown that these blood stem cells (often used in bone marrow transplants) couldn't be grown outside the body unless MSC's were present.
You see, MSC's live in a "stem cell niche". In the bone marrow, this niche contains many other cells. There is evidence of chemical communication between MSC's and these other cells. Why? When we examined that question in 2005, it seemed logical that if MSC's had to be present to help other cells live outside the body, this would be a two way street. These other cells must have the ability to help MSC's. As a result, we coined the term, "Progenitor Helper Cells" (PHC's), for all of the other cells that assist MSC's.
In 2005, it only seemed a matter of time before we would understand how all the other cells in this stem cell niche helped MSC's get their work done. As it happens, research is now proving this concept. In one study published this week, MSC's and bone marrow cells were both needed to repair a rat pancreas in a diabetic mouse. This is a big deal, in that it means that the traditional concept of culturing MSC's in isolation and deploying them in isolation may be concept that isn't as effective as using the cells in a more natural way (meaning MSC's and PHC's together).
In summary, we believe that MSC's work with these other cells to act as "construction managers", overseeing or managing various parts of the repair processes. So it seems that "it takes a village" to both raise children and repair tissues.
Sunday, October 14, 2007
Wednesday, October 10, 2007
Latest MSC News
As a stem cell researcher, the term "MSC" means, mesenchymal stem cell. For more information on these cells, see http://youtube.com/watch?v=WaRnVcwZ0i8.
MSC's are again showing up in the U.S. National Library of Medicine database. Some exciting stuff:
-Two rat models showing that these cells can reduce the size of dead brain tissue in both embolic and hemorrhagic stroke. Embolic stroke is where a blood clot makes it's way to the brain and shuts off some of the blood supply to the brain. It's the most common type of stroke. This is a big deal, since the cells were given via IV, an easy way to get cells into the body. What might this look like in the future? A patient has the signs and symptoms of stroke and is seen in the ER. The same clot busting drugs now used to open the area are given to the patient (to restore blood flow), but these drugs are also followed by an infusion of the patent's stem cells (stored on ice in a storage facility). This allows the damage caused by the blot clot to be more limited and helps the damaged area heal. As a result, what could have been a tragedy is now limited to a bad day.
This again underscores that storing your cells for future use is likely to be a big deal in the future. One of the problems with using another person's cells is the fact that recent research shows that it may be possible to transmit genetic diseases (see http://stemcells.alphamedpress.org/cgi/content/abstract/25/6/1356). This study showed that it was possible to give osteoporosis to a normal young mouse by transplanting stem cells from an old mouse with osteoporosis. The moral of that story? Until we know how to screen for all known genetic diseases, use your own cells!
MSC's are again showing up in the U.S. National Library of Medicine database. Some exciting stuff:
-Two rat models showing that these cells can reduce the size of dead brain tissue in both embolic and hemorrhagic stroke. Embolic stroke is where a blood clot makes it's way to the brain and shuts off some of the blood supply to the brain. It's the most common type of stroke. This is a big deal, since the cells were given via IV, an easy way to get cells into the body. What might this look like in the future? A patient has the signs and symptoms of stroke and is seen in the ER. The same clot busting drugs now used to open the area are given to the patient (to restore blood flow), but these drugs are also followed by an infusion of the patent's stem cells (stored on ice in a storage facility). This allows the damage caused by the blot clot to be more limited and helps the damaged area heal. As a result, what could have been a tragedy is now limited to a bad day.
This again underscores that storing your cells for future use is likely to be a big deal in the future. One of the problems with using another person's cells is the fact that recent research shows that it may be possible to transmit genetic diseases (see http://stemcells.alphamedpress.org/cgi/content/abstract/25/6/1356). This study showed that it was possible to give osteoporosis to a normal young mouse by transplanting stem cells from an old mouse with osteoporosis. The moral of that story? Until we know how to screen for all known genetic diseases, use your own cells!
Subscribe to:
Posts (Atom)